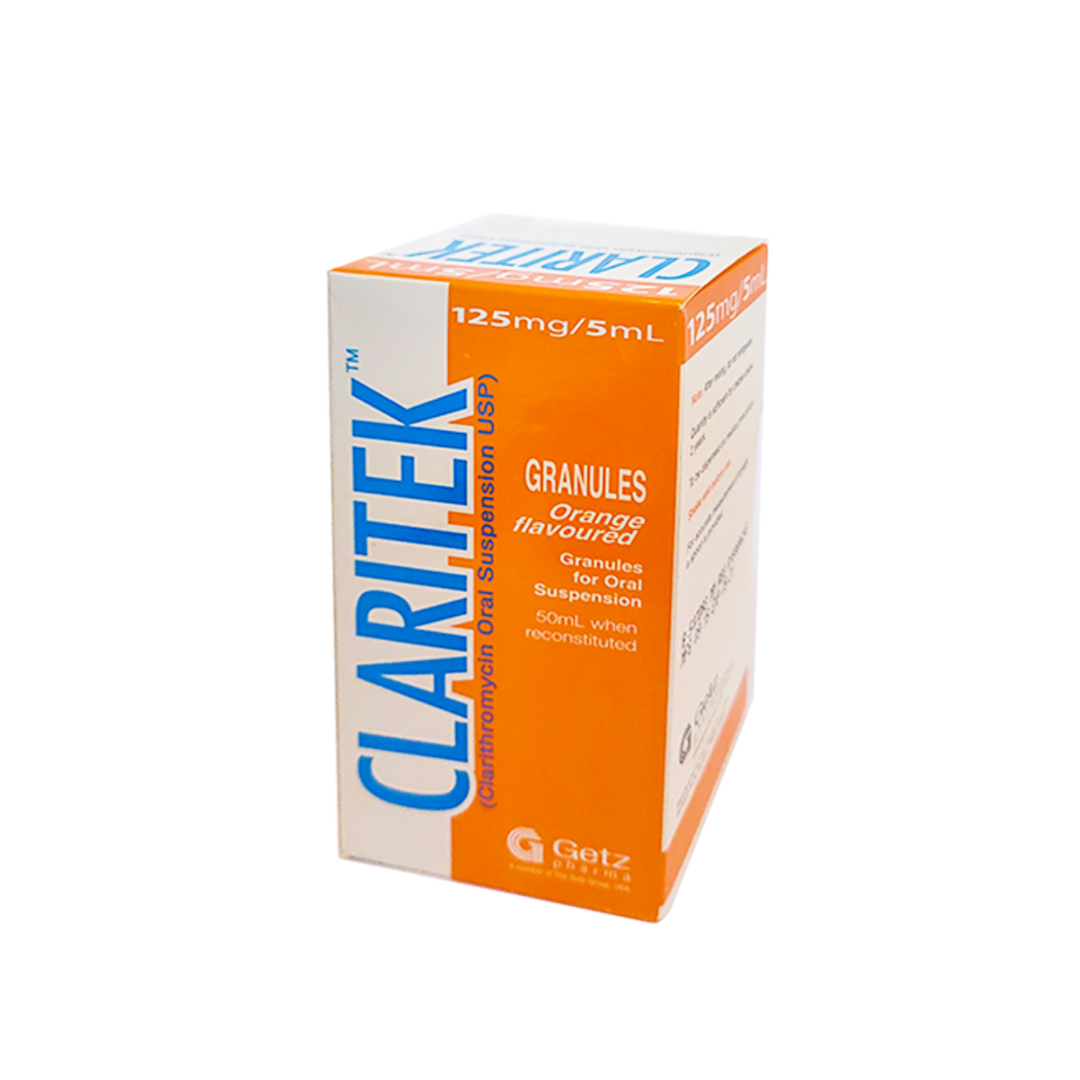
CLARITEK SYRUP 125mg / 5ml
Rs. 499.00
|
Unit : 1 |
Brand : Getz Pharma |
| Age group : NULL |
Location:
NULL
Material:
NULL
Item Details
Prescription Needed (Rx)| Drug Form: | Suspension |
|---|---|
| Storage Temperature: | NULL |
| Administration Method: | NULL |
| Presentation: | NULL |
Generic Details: Clarithromycin
| Generic Name: | Clarithromycin View Generic Items |
|---|---|
| Main Drug Group: | macrolide antibiotics |
| Indication: | it is an antibiotic used to treat various bacterial infections. This includes strep throat, pneumonia, skin infections, H. pylori infection, and Lyme disease, among others. |
| Dosage: | Usual Adult Dose for Tonsillitis/Pharyngitis Immediate-release: 250 mg orally every 12 hours for 10 days Comments: -The drug of choice for treatment and prevention of streptococcal infections and prophylaxis of rheumatic fever is IM or oral penicillin. -In general, this drug effectively eradicates Streptococcus pyogenes from the nasopharynx; efficacy in the subsequent prevention of rheumatic fever has not been established. Use: For the treatment of pharyngitis/tonsillitis due to S pyogenes Usual Adult Dose for Sinusitis Immediate-release: 500 mg orally every 12 hours for 14 days Extended-release: 1000 mg orally every 24 hours for 14 days Uses: For the treatment of acute maxillary sinusitis due to Haemophilus influenzae, Moraxella catarrhalis, or S pneumoniae Usual Adult Dose for Bronchitis Immediate-release: -Due to H influenzae: 500 mg orally every 12 hours for 7 to 14 days -Due to H parainfluenzae: 500 mg orally every 12 hours for 7 days -Due to M catarrhalis or S pneumoniae: 250 mg orally every 12 hours for 7 to 14 days Extended-release: 1000 mg orally every 24 hours for 7 days Uses: For the treatment of acute bacterial exacerbation of chronic bronchitis due to H influenzae, H parainfluenzae, M catarrhalis, or S pneumoniae Usual Adult Dose for Pneumonia Immediate-release: -Due to H influenzae: 250 mg orally every 12 hours for 7 days -Due to S pneumoniae or Chlamydophila pneumoniae: 250 mg orally every 12 hours for 7 to 14 days Extended-release: 1000 mg orally every 24 hours for 7 days Uses: For the treatment of community-acquired pneumonia due to: -Immediate-release: H influenzae, S pneumoniae, or C pneumoniae (TWAR) -Extended-release: H influenzae, H parainfluenzae, M catarrhalis, S pneumoniae, C pneumoniae (TWAR) Usual Adult Dose for Mycoplasma Pneumonia Immediate-release: 250 mg orally every 12 hours for 7 to 14 days Extended-release: 1000 mg orally every 24 hours for 7 days Use: For the treatment of community-acquired pneumonia due to Mycoplasma pneumoniae Usual Adult Dose for Skin and Structure Infection Immediate-release: 250 mg orally every 12 hours for 7 to 14 days Comments: -Abscesses usually require surgical drainage. Uses: For the treatment of uncomplicated skin and skin structure infections due to Staphylococcus aureus or S pyogenes Usual Adult Dose for Helicobacter pylori Infection Immediate-release: Triple therapy: -In combination with lansoprazole and amoxicillin: Clarithromycin 500 mg orally every 12 hours for 10 to 14 days -In combination with omeprazole and amoxicillin: Clarithromycin 500 mg orally every 12 hours for 10 days Dual therapy: -In combination with omeprazole: Clarithromycin 500 mg orally every 8 hours for 14 days -In combination with ranitidine bismuth citrate: Clarithromycin 500 mg orally every 8 to 12 hours for 14 days Comments: -Helicobacter pylori eradication shown to reduce the risk of duodenal ulcer recurrence -Regimens with this drug as the only antimicrobial agent are more likely to be associated with clarithromycin resistance in patients who fail therapy. -Regimens containing this drug should not be used in patients with known or suspected clarithromycin-resistant isolates; efficacy of therapy is reduced. -Susceptibility testing is recommended in patients who fail therapy; if resistance to this drug is established, a non-clarithromycin-containing regimen is recommended. -The manufacturer product information for the other drugs indicated in combination with clarithromycin should be consulted. Uses: -Triple therapy: In combination with amoxicillin and (lansoprazole or omeprazole), for the treatment of patients with H pylori infection and duodenal ulcer disease (active or 5-year history of duodenal ulcer) to eradicate H pylori -Dual therapy: In combination with omeprazole or ranitidine bismuth citrate, for the treatment of patients with active duodenal ulcer associated with H pylori infection Usual Adult Dose for Mycobacterium avium-intracellulare - Prophylaxis Immediate-release: 500 mg orally twice a day Use: For the prevention of disseminated Mycobacterium avium complex (MAC) disease in patients with advanced HIV infection US CDC, National Institutes of Health (NIH), and HIV Medicine Association of the Infectious Diseases Society of America (HIVMA/IDSA) Recommendations for HIV-infected Patients: -Primary prevention of disseminated MAC disease: 500 mg orally twice a day -Chronic maintenance therapy (secondary prophylaxis) for disseminated MAC disease: 500 mg orally twice a day Comments: -Primary prophylaxis against disseminated MAC disease recommended for patients with CD4 count less than 50 cells/mm3 (after active disseminated MAC disease has been ruled out based on clinical assessment). -This drug is a preferred prophylactic agent for primary prevention of disseminated MAC disease (except during pregnancy). -The combination of this drug and rifabutin should not be used for primary MAC prophylaxis; not more effective than this drug alone. -Primary MAC prophylaxis should be discontinued in patients responding to antiretroviral therapy (ART) with increase in CD4 count to greater than 100 cells/mm3 for at least 3 months; should restart if CD4 count declines to less than 50 cells/mm3. -This drug should be used with ethambutol for chronic maintenance therapy; same regimen as for treatment. -Patients with disseminated MAC disease should continue chronic maintenance therapy (secondary prophylaxis) unless immune reconstitution occurs due to ART. -Chronic maintenance therapy may be stopped in patients at low risk of MAC recurrence; such patients have completed at least 12 months of MAC therapy, have no signs/symptoms of MAC disease, and have an increase in CD4 count to greater than 100 cells/mm3 for more than 6 months in response to ART; should restart if CD4 count declines to less than 100 cells/mm3. Usual Adult Dose for Mycobacterium avium-intracellulare - Treatment Immediate-release: 500 mg orally twice a day Comments: -Recommended as the primary agent for the treatment of disseminated infection due to MAC -This drug should be used in combination with other antimycobacterial agents that have shown in vitro activity against MAC or clinical benefit in MAC treatment. -Therapy should continue if clinical response is observed; can discontinue this drug when patient considered at low risk of disseminated infection. Uses: For the treatment of disseminated mycobacterial infections due to M avium or M intracellulare US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-infected Patients: -Treatment of disseminated MAC disease: 500 mg orally twice a day Comments: -This drug should be used with ethambutol. -Combination therapy with at least 2 antimycobacterial drugs is recommended for initial treatment of MAC disease to prevent/delay resistance development. -This drug is the preferred first agent (except during pregnancy); ethambutol is the recommended second agent. -Addition of a third or fourth agent should be considered for patients with CD4 count less than 50 cells/mm3, high mycobacterial loads, or when effective ART is absent; some experts recommend rifabutin as a third agent. -MAC isolates should be tested for susceptibility to this drug in all patients. -Patients with disseminated MAC disease should continue chronic maintenance therapy (secondary prophylaxis) unless immune reconstitution occurs due to ART. Usual Adult Dose for Bacterial Endocarditis Prophylaxis American Heart Association (AHA) recommendations: Immediate-release: 500 mg orally as a single dose 30 to 60 minutes before procedure Comments: -Recommended for patients allergic to penicillins Usual Adult Dose for Legionella Pneumonia Some experts recommend: Immediate-release: 500 mg orally every 12 hours Duration of therapy: -For mild to moderate infections in immunocompetent patients: 10 days -To prevent relapse, especially in patients with more severe infections or with underlying comorbidity or immunodeficiency: 3 weeks may be necessary Comments: -Recommended for Legionnaires' disease Usual Adult Dose for Pertussis Prophylaxis US CDC recommendations: Immediate-release: 500 mg orally every 12 hours for 7 days Comments: -Recommended for treatment and postexposure prophylaxis -Macrolides are preferred agents for the treatment of pertussis. Usual Adult Dose for Pertussis US CDC recommendations: Immediate-release: 500 mg orally every 12 hours for 7 days Comments: -Recommended for treatment and postexposure prophylaxis -Macrolides are preferred agents for the treatment of pertussis. Usual Pediatric Dose for Tonsillitis/Pharyngitis Immediate-release: 6 months or older: 7.5 mg/kg orally every 12 hours for 10 days Maximum dose: 500 mg/dose Uses: For the treatment of pharyngitis/tonsillitis due to S pyogenes Usual Pediatric Dose for Sinusitis Immediate-release: 6 months or older: 7.5 mg/kg orally every 12 hours for 10 days Maximum dose: 500 mg/dose Uses: For the treatment of acute maxillary sinusitis due to H influenzae, M catarrhalis, or S pneumoniae Usual Pediatric Dose for Mycoplasma Pneumonia Immediate-release: 6 months or older: 7.5 mg/kg orally every 12 hours for 10 days Maximum dose: 500 mg/dose Uses: For the treatment of community-acquired pneumonia due to M pneumoniae, S pneumoniae, or C pneumoniae (TWAR) Usual Pediatric Dose for Pneumonia Immediate-release: 6 months or older: 7.5 mg/kg orally every 12 hours for 10 days Maximum dose: 500 mg/dose Uses: For the treatment of community-acquired pneumonia due to M pneumoniae, S pneumoniae, or C pneumoniae (TWAR) Usual Pediatric Dose for Otitis Media Immediate-release: 6 months or older: 7.5 mg/kg orally every 12 hours for 10 days Maximum dose: 500 mg/dose Uses: For the treatment of acute otitis media due to H influenzae, M catarrhalis, or S pneumoniae Usual Pediatric Dose for Skin and Structure Infection Immediate-release: 6 months or older: 7.5 mg/kg orally every 12 hours for 10 days Maximum dose: 500 mg/dose Comments: -Abscesses usually require surgical drainage. Uses: For the treatment of uncomplicated skin and skin structure infections due to S aureus or S pyogenes Usual Pediatric Dose for Mycobacterium avium-intracellulare - Prophylaxis Immediate-release: 20 months or older: 7.5 mg/kg orally twice a day Maximum dose: 500 mg/dose Use: For the prevention of disseminated MAC disease in patients with advanced HIV infection US CDC, NIH, HIVMA/IDSA, Pediatric Infectious Diseases Society (PIDS), and American Academy of Pediatrics (AAP) Recommendations for HIV-exposed and HIV-infected Children: -Primary prevention of MAC infections: 7.5 mg/kg orally twice a day -Chronic suppressive therapy for MAC infections: 7.5 mg/kg orally twice a day Maximum dose: 500 mg/dose Comments: -Primary prophylaxis recommended for patients aged 6 years or older with CD4 count less than 50 cells/mm3, aged 2 to less than 6 years with CD4 count less than 75 cells/mm3, aged 1 to less than 2 years with CD4 count less than 500 cells/mm3, and aged less than 1 year with CD4 count less than 750 cells/mm3. -Before prophylaxis is started, active disseminated MAC disease should be ruled out based on clinical assessment. -Primary prophylaxis can be discontinued in patients 2 years or older if they have received stable combination ART (cART) for at least 6 months and have sustained an increase in CD4 count well above the age-specific target for starting prophylaxis (e.g., greater than 100 cells/mm3 for patients aged 6 years or older; greater than 200 cells/mm3 for patients aged 2 to less than 6 years) for longer than 3 months; specific recommendations for discontinuing MAC prophylaxis in patients younger than 2 years have not been established. -This drug should be used with ethambutol (with or without rifabutin) for chronic suppressive therapy. -To prevent recurrence, lifelong prophylaxis is recommended for children with history of disseminated MAC. -Some experts recommend stopping chronic suppressive therapy in patients 2 years or older who have completed at least 12 months of MAC therapy, who have no signs/symptoms of MAC disease, who receive stable cART, and who have sustained an increase in CD4 count well above the age-specific target for starting primary prophylaxis (e.g., greater than 100 cells/mm3 for patients 6 years or older; greater than 200 cells/mm3 for patients aged 2 to less than 6 years) for at least 6 months; should restart if CD4 count falls below age-specific targets. US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-infected Adolescents: -Primary prevention of disseminated MAC disease: 500 mg orally twice a day -Chronic maintenance therapy (secondary prophylaxis) for disseminated MAC disease: 500 mg orally twice a day Comments: -Primary prophylaxis against disseminated MAC disease recommended for patients with CD4 count less than 50 cells/mm3 (after active disseminated MAC disease has been ruled out based on clinical assessment). -This drug is a preferred prophylactic agent for primary prevention of disseminated MAC disease (except during pregnancy). -The combination of this drug and rifabutin should not be used for primary MAC prophylaxis; not more effective than this drug alone. -Primary MAC prophylaxis should be discontinued in patients responding to ART with increase in CD4 count to greater than 100 cells/mm3 for at least 3 months; should restart if CD4 count declines to less than 50 cells/mm3. -This drug should be used with ethambutol for chronic maintenance therapy; same regimen as for treatment. -Patients with disseminated MAC disease should continue chronic maintenance therapy (secondary prophylaxis) unless immune reconstitution occurs due to ART. -Chronic maintenance therapy may be stopped in patients at low risk of MAC recurrence; such patients have completed at least 12 months of MAC therapy, have no signs/symptoms of MAC disease, and have an increase in CD4 count to greater than 100 cells/mm3 for more than 6 months in response to ART; should restart if CD4 count declines to less than 100 cells/mm3. Usual Pediatric Dose for Mycobacterium avium-intracellulare - Treatment Immediate-release: 20 months or older: 7.5 mg/kg orally twice a day Maximum dose: 500 mg/dose Comments: -Recommended as the primary agent for the treatment of disseminated infection due to MAC -This drug should be used in combination with other antimycobacterial agents that have shown in vitro activity against MAC or clinical benefit in MAC treatment. -Therapy should continue if clinical response is observed; can discontinue this drug when patient considered at low risk of disseminated infection. Uses: For the treatment of disseminated mycobacterial infections due to M avium or M intracellulare US CDC, NIH, HIVMA/IDSA, PIDS, and AAP Recommendations for HIV-exposed and HIV-infected Children: -Treatment of MAC infections: 7.5 to 15 mg/kg orally twice a day Maximum dose: 500 mg/dose Comments: -This drug should be used with ethambutol (with or without rifabutin). -Combination therapy with at least 2 antimycobacterial drugs is recommended to prevent/delay resistance development. -Some experts use this drug as the preferred first agent; ethambutol is the recommended second agent; some experts recommend rifabutin as a third agent for severe disease. -MAC isolates should be tested for susceptibility to this drug. -Chronic suppressive therapy (secondary prophylaxis) is recommended after initial therapy. US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-infected Adolescents: -Treatment of disseminated MAC disease: 500 mg orally twice a day Comments: -This drug should be used with ethambutol. -Combination therapy with at least 2 antimycobacterial drugs is recommended for initial treatment of MAC disease to prevent/delay resistance development. -This drug is the preferred first agent (except during pregnancy); ethambutol is the recommended second agent. -Addition of a third or fourth agent should be considered for patients with CD4 count less than 50 cells/mm3, high mycobacterial loads, or when effective ART is absent; some experts recommend rifabutin as a third agent. -MAC isolates should be tested for susceptibility to this drug in all patients. -Patients with disseminated MAC disease should continue chronic maintenance therapy (secondary prophylaxis) unless immune reconstitution occurs due to ART. Usual Pediatric Dose for Pertussis Prophylaxis US CDC recommendations: Immediate-release: 1 month or older: 7.5 mg/kg orally every 12 hours for 7 days Maximum dose: 500 mg/dose Comments: -Recommended for treatment and postexposure prophylaxis -Macrolides are preferred agents for the treatment of pertussis. Usual Pediatric Dose for Pertussis US CDC recommendations: Immediate-release: 1 month or older: 7.5 mg/kg orally every 12 hours for 7 days Maximum dose: 500 mg/dose Comments: -Recommended for treatment and postexposure prophylaxis -Macrolides are preferred agents for the treatment of pertussis. Usual Pediatric Dose for Bacterial Endocarditis Prophylaxis AHA recommendations: Immediate-release: 15 mg/kg orally as a single dose 30 to 60 minutes before procedure Maximum dose: 500 mg/dose Comments: -Recommended for children allergic to penicillins |
| Pregnancy Category: | C |
Features & Specifications
NULL














